Sleep Disorders Taree
- Clinician-reviewed sleep disorder diagnostics
- Personalised treatment backed by data
- CPAP therapy supported by ongoing care
CPAP & Treatment Services
The most effective way to treat Obstructive Sleep Apnoea (OSA) is with CPAP (Continuous Positive Airway Pressure) or APAP (Automatic Positive Airway Pressure). Most sleep physicians recommend a trial of CPAP or APAP before pursuing other forms of treatment. It can be used in patients with mild, moderate or severe sleep apnoea.
CPAP/APAP therapy does not cure obstructive sleep apnoea; therefore, it must be used every night while you are sleeping. If you stop using CPAP/APAP therapy, your symptoms will return, and you will start snoring and having apnoea’s again.
Some of the benefits in treating sleep apnoea include:
- Cessation of snoring
- Reduction in cardiovascular events, such as heart attack & stroke
- Reduced risk of having a motor vehicle accident or workplace accident
- Reduction in daytime sleepiness
- Improved concentration & memory
- Reduction in morning headaches
- Waking up feeling more refreshed
How Does CPAP Work?
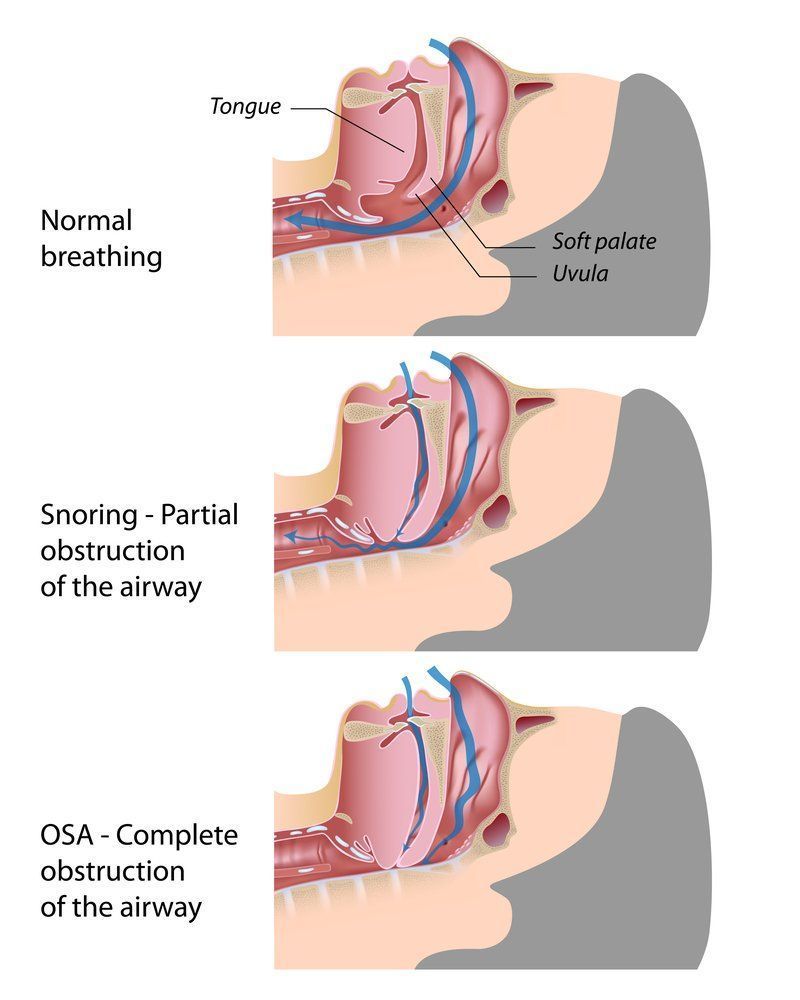
The pressure from CPAP/APAP therapy is delivered continuously during the night while you sleep. When the correct pressure is applied via a small mask, the airway is sufficiently opened to allow regular unobstructed breathing, thereby controlling apnoea events and snoring. The body’s oxygen levels remain stable, and sleep is no longer disrupted. A CPAP/APAP machine only opens your airway and does not breathe for you or supply oxygen.
CPAP machines deliver one constant pressure throughout the night, whereas APAP machines are set to deliver varying pressures while you sleep and can self-adjust when apnoea events occur.
In the past, these machines were large and noisy, but now, with greater advancements in technology, they are small and quiet with many comfort features integrated into the machines.
CPAP Rental & Trial
After your home sleep study, and your doctor has recommended you commence a trial of CPAP treatment, the next step is to make an appointment at one of our clinics to commence treatment.
The CPAP trial period is usually between four to six weeks, which allows you time to become used to the machine and mask and feel the benefits of treatment. Our highly trained CPAP therapists will monitor and support you through this trial period by either in-clinic or phone consultations, which uses remote access to your hired device.
We use the most up-to-date machines and masks available from leading companies, which means you have access to the most recent advancements in the field. The hire fee covers all consultations within the trial period, along with all the equipment hired during this time.
At the end of the CPAP trial, you can decide whether you have felt an improvement in your sleep quality and general well-being, and therefore wish to continue treatment by purchasing your own equipment from one of our clinics.
All our CPAP therapists are experienced and highly trained. They will support and guide you through your treatment and provide you with education and follow-up care. You can book an appointment with our CPAP therapists by contacting us.
Snoring
Snoring occurs when the soft tissue in the back of your throat relaxes too much and starts to vibrate. The sound from this vibration can become loud and disruptive. Chronic loud snoring can be an indication of a more serious sleep problem, such as Obstructive Sleep Apnoea. If you snore loudly with episodes of stopping breathing and frequent sleep arousals, you may have OSA.
You are more likely to snore if you are:
- Overweight or obese: Carrying extra fatty tissue, especially around the neck area, can increase the restriction of your airway when the muscles in your throat relax.
- A male: Men are at higher risk of OSA than women. Middle-aged men often carry more weight, which can accumulate around the neck and jaw, putting added pressure on the airway during sleep.
- Older: As we grow older, we tend to lose muscle tone, including in the upper airway.
- Drinking alcohol: Alcohol is a muscle relaxant, so while you are sleeping this will increase the length and noise of your snoring. Taking sleeping tablets or sedatives to help you sleep. Sleeping tablets can also make snoring worse as the medication will relax the muscles in the back of your airway even more.
- Going through menopause: As women go through menopause the level of oestrogen drops, which results in poorer muscle tone, including in the upper airway. Thereby it increases the incidence of snoring.
To learn about alternative treatments for OSA, get in touch.
Insomnia
Insomnia is a common and distressing sleep disorder which can become chronic if untreated. If you regularly find it hard to fall asleep or stay asleep, then this can be your first sign of insomnia. It is usually associated with daytime tiredness and distress. If these symptoms last more than a month, you may have chronic insomnia.
Where can I find out more?
https://www.sleepfoundation.org/insomnia
https://www.woolcock.org.au/insomnia-research
A Mindful Way is an Australian, six-week digital online self-help program that teaches mindfulness and cognitive-behavioural skills for sleep improvement at a cost. A Monash University randomised control pilot study showed completion of the program led to significant improvement in measures of insomnia. (This link is provided for information only and is not an endorsement of their products and services).
Leg Movement Disorders
What is PLMS?
Periodic Limb Movements of Sleep (PLMS) is the movement of legs or arms every 10 to 60 seconds while the patient is asleep. It is out of your control and mainly appears during the deepest type of sleep in the first third of the night. PLMS can happen in several ways, including flexing toes or feet, bending ankles or knees and twitching the hip. It tends to reoccur as well.
Often, the way people discover that they have PLMS is when their bed partner complains of being kicked or the blankets are jumbled in the morning. In some cases, PLMS can disrupt the sleep of the patient or that of their bed partner. If it’s a problem, we recommend treatment.
Where can I get further information?
https://www.emedicinehealth.com/periodic_limb_movement_disorder/article_em.htm
https://sleepeducation.org/sleep-disorders/periodic-limb-movements/
What is RLS?
RLS is where you experience significant discomfort in your limbs. People describe it as tingling, itching, prickly and painful sensations. It generally affects the legs more than the arms. When it happens, you’ll feel a strong or irresistible urge to move the affected limbs.
RLS can occur when sitting for long periods, such as at a desk, travelling in a vehicle or plane and watching a movie. It may also affect you when you lie down to sleep. RLS is worse in the evenings, making it difficult to fall asleep. If you do get to sleep, you might wake up multiple times during the night. Eventually, you can feel irritable, anxious and depressed.
Where can I get further information?
https://www.helpguide.org/articles/sleep/restless-leg-syndrome-rls.htm
Frequently Asked Questions
What are the most common types of sleep disorders?
There are more than 80 recognised sleep disorders, but the most common include obstructive sleep apnoea, insomnia, restless legs syndrome (RLS), narcolepsy, and circadian rhythm disorders. Obstructive sleep apnoea causes breathing to stop and start repeatedly during sleep, often due to airway collapse. Insomnia is characterised by difficulty falling asleep, staying asleep, or waking too early. RLS involves uncomfortable sensations in the legs, usually at night, leading to an irresistible urge to move them. Narcolepsy causes excessive daytime sleepiness and sudden sleep attacks, while circadian rhythm disorders disrupt the internal sleep-wake cycle, often due to shift work or irregular schedules. Each condition presents with different symptoms and requires specific diagnosis and treatment strategies.
What causes sleep disorders?
Sleep disorders can be caused by a variety of factors including medical conditions, lifestyle habits, psychological issues, and genetic predisposition. For example, obstructive sleep apnoea is often linked to physical factors such as enlarged tonsils, obesity, or a recessed jaw. Insomnia may be triggered by stress, anxiety, depression, or the use of stimulants like caffeine or certain medications. Restless legs syndrome is believed to have a neurological basis and may be hereditary or related to iron deficiency. Narcolepsy is thought to involve autoimmune responses affecting the brain's regulation of sleep. Environmental influences, irregular sleep schedules, and poor sleep hygiene can also contribute to the development or worsening of sleep disorders.
How do I know if I have a sleep disorder?
Common signs of a sleep disorder include loud snoring, gasping for air during sleep, frequent nighttime awakenings, difficulty falling or staying asleep, excessive daytime sleepiness, and trouble concentrating or remembering things. Some people also report mood changes, morning headaches, or a dry mouth upon waking. If these symptoms occur regularly and interfere with daily functioning, it’s a strong indication that a sleep disorder may be present. Diagnosis typically involves a clinical consultation and, in many cases, a sleep study to monitor breathing, heart rate, oxygen levels, and brain activity during sleep.